Many within the deliverance ministry would categorize sudden shifts in behavior as having demonic influence. Before reaching this conclusion, we must first consider physical causation.
I deal with deliverance ministry. When a Christian (or non-believer) comes to me with a problem area, I conduct multiple interviews to narrow down the symptoms. While we do not wrestle against flesh and blood, in most cases, a person’s body works against them. It is with this idea that I would like to discuss Glioblastoma.
Introduction
Glioblastoma, also known as glioblastoma multiforme (GBM), is an aggressive type of brain tumor that arises from astrocytes, the star-shaped cells that make up the brain’s supportive tissue. It is classified as a grade IV astrocytoma, indicating its highly malignant nature. Glioblastomas are notorious for their rapid growth, resistance to treatment, and poor prognosis, making them a significant focus of neurological and oncological research. This report provides an in-depth overview of glioblastoma, covering its characteristics, symptoms, diagnosis, treatment, prognosis, insights into personality changes, and the sudden onset of symptoms.
Characteristics of Glioblastoma
Glioblastomas are the most common and aggressive primary malignant brain tumors in adults. They account for about 15% of all primary brain and central nervous system (CNS) tumors and approximately 48% of malignant brain tumors (American Brain Tumor Association). The annual incidence of glioblastoma in the United States is about 3.19 per 100,000 people, translating to roughly 13,000 to 14,000 new cases yearly (Ostrom et al.).
Aggressiveness
Glioblastomas are characterized by rapid growth and invasiveness. They infiltrate nearby brain tissue, making complete surgical removal nearly impossible. This aggressive behavior is driven by genetic mutations that lead to uncontrolled cell proliferation and resistance to apoptosis (programmed cell death).
Symptoms
The symptoms of glioblastoma vary depending on the tumor’s location in the brain. Common symptoms include:
- Headaches: Often worse in the morning and may be accompanied by nausea and vomiting.
- Seizures: New onset of seizures in an adult is a common initial sign.
- Neurological Deficits: Sudden weakness or numbness in limbs, difficulty with speech, vision problems, or balance issues.
- Cognitive and Personality Changes: Sudden changes in mood, personality, or cognitive abilities, including memory loss and confusion.
Diagnosis
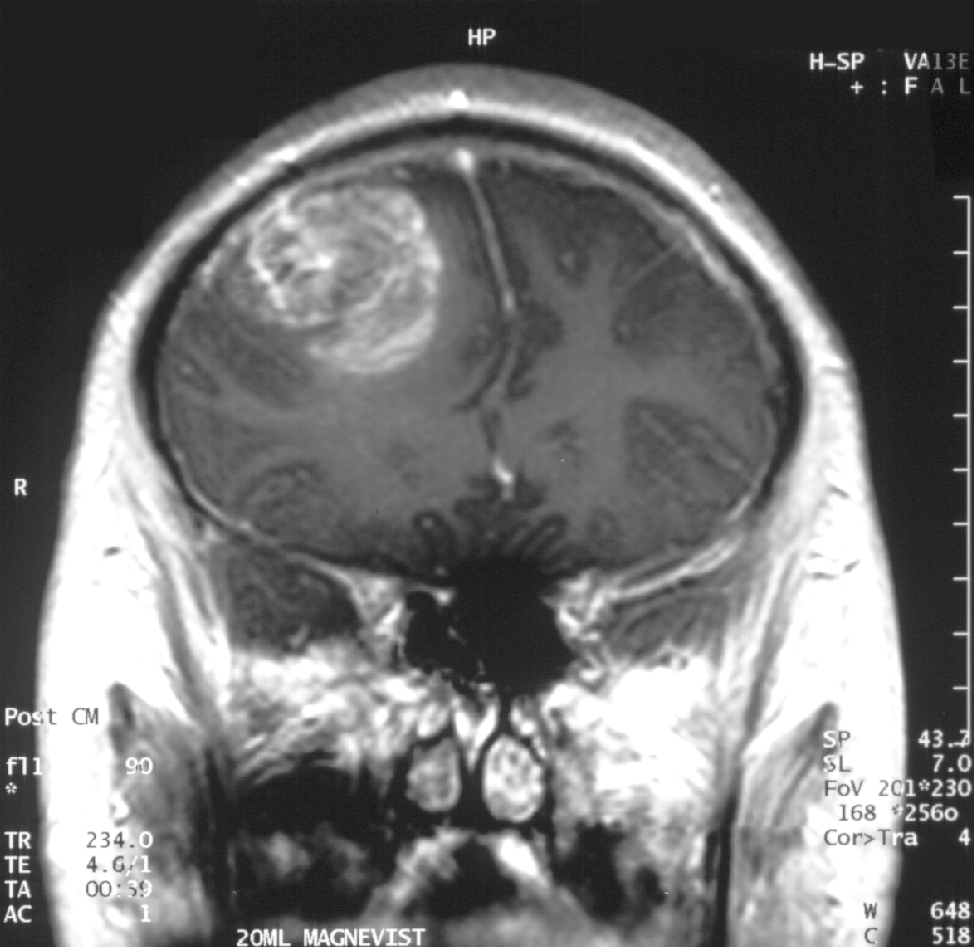
Diagnosis of glioblastoma typically involves imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans. A definitive diagnosis is made through a biopsy, where a tissue sample is examined under a microscope. Advanced imaging techniques, such as functional MRI and positron emission tomography (PET), may also be used to assess the tumor’s extent and activity.
Treatment
Treatment options for glioblastoma are limited and primarily aim to prolong survival and alleviate symptoms rather than cure the disease. Standard treatments include:
- Surgery: To remove as much of the tumor as possible.
- Radiation Therapy: To target and kill remaining cancer cells post-surgery.
- Chemotherapy: Often with the drug temozolomide, which can cross the blood-brain barrier.
- Targeted Therapy: Such as bevacizumab, which inhibits the growth of blood vessels that supply the tumor.
- Experimental Therapies: Including clinical trials investigating new drugs, immunotherapy, and gene therapy.
Prognosis
The prognosis for glioblastoma is generally poor, with median survival time typically around 12-15 months following diagnosis, even with aggressive treatment. Factors such as patient age, overall health, and the tumor’s genetic characteristics can influence individual outcomes.
Personality Changes in Glioblastoma Patients
Personality changes are common in individuals with glioblastoma, particularly when the tumor affects the frontal lobes of the brain. These changes can be distressing for both the patient and their loved ones.
Mechanisms of Personality Changes
- Direct Tumor Effects: The tumor itself can disrupt normal brain activity by compressing, invading, or destroying brain tissue, leading to alterations in behavior and personality.
- Increased Intracranial Pressure: As the tumor grows, it can increase pressure within the skull, affecting brain function and potentially leading to changes in personality.
- Treatment Side Effects: Treatments such as surgery, radiation therapy, and chemotherapy can also impact brain function, contributing to personality changes.
Common Personality Changes
- Emotional Lability: Patients may experience rapid mood swings and heightened emotional responses, including irritability, anger, or inappropriate laughter or crying.
- Apathy and Withdrawal: A reduction in interest in activities and social interactions, leading to social withdrawal and a lack of motivation.
- Cognitive Changes: Difficulties with concentration, memory, and decision-making can impact behavior, leading to frustration and changes in how individuals interact with others.
- Depression and Anxiety: The stress and emotional burden of the diagnosis and treatment can lead to depression and anxiety, which may further affect personality and behavior.
- Disinhibition: Reduced ability to control impulses, leading to socially inappropriate behavior, lack of restraint, or reckless actions.
- Aggressiveness: Some patients may become more aggressive or confrontational, which can be distressing for family members and caregivers.
Disinhibition: Examples and Impact
Disinhibition is a significant symptom for individuals with glioblastoma, particularly when the tumor affects the frontal lobes. Examples of disinhibited behaviors include:
- Inappropriate Social Behavior: Making rude or tactless comments, engaging in socially unacceptable behavior, and invading others’ personal space.
- Impulsivity: Acting without thinking, making hasty decisions or purchases, and interrupting conversations frequently.
- Sexual Inappropriateness: Making inappropriate sexual remarks or advances and engaging in public displays of affection that are not socially acceptable.
- Lack of Restraint in Emotional Expression: Displaying exaggerated emotions, such as laughing or crying uncontrollably.
- Neglect of Personal Hygiene and Appearance: Ignoring social norms related to cleanliness, grooming, and dressing appropriately.
- Financial Recklessness: Spending money irresponsibly, such as gambling or making large, unnecessary purchases.
- Inappropriate Humor: Making jokes or offensive or inappropriate comments for the context.
Disinhibited behaviors can strain relationships with family, friends, and colleagues, as others may find it difficult to understand or tolerate these sudden changes in behavior. These behaviors can also lead to social isolation and difficulties in maintaining employment or engaging in social activities.
Management of Personality Changes
- Behavioral Interventions include setting clear boundaries, providing gentle reminders about appropriate behavior, and using positive reinforcement to encourage desirable behaviors.
- Environmental Modifications: Creating a structured environment with consistent routines to reduce opportunities for impulsive behavior and minimizing exposure to situations that may trigger inappropriate behavior.
- Medications: Antidepressants, antipsychotics, or mood stabilizers may help manage symptoms of disinhibition.
- Therapeutic Support: Counseling or therapy for the patient and family to develop coping strategies and neuropsychological rehabilitation to improve cognitive function and self-control.
Sudden Onset of Symptoms
Glioblastoma is typically a rapidly progressing disease, and its symptoms can suddenly appear. However, the development of the tumor itself is a gradual process that occurs over time before symptoms become noticeable.
Gradual Development vs. Sudden Onset
- Gradual Tumor Growth: Glioblastoma develops due to genetic mutations in brain cells, leading to uncontrolled cell growth. This process can take months or even years. Initially, the tumor may grow silently without causing noticeable symptoms.
- Sudden Onset of Symptoms: Despite the gradual growth of the tumor, symptoms often appear suddenly and progress rapidly. This sudden onset is due to the tumor reaching a size or location where it starts to interfere significantly with brain function. Factors that contribute to the sudden appearance of symptoms include:
- Tumor Size: As the tumor grows, it increases intracranial pressure, which can lead to headaches, nausea, and vomiting.
- Location: Tumors in critical brain areas can quickly affect motor functions, speech, vision, or personality.
- Edema: The tumor may cause swelling (edema) in the brain, exacerbating symptoms suddenly.
- Bleeding: Occasionally, glioblastomas can bleed (hemorrhage), leading to a sudden worsening of symptoms.
Common Sudden Symptoms
- Headaches: Often worse in the morning and may be accompanied by nausea and vomiting.
- Seizures: A new onset of seizures in an adult is a common initial sign.
- Neurological Deficits: Sudden weakness or numbness in limbs, difficulty with speech, vision problems, or balance issues.
- Cognitive and Personality Changes: Sudden changes in mood, personality, or cognitive abilities, including memory loss and confusion.
Diagnosis and Immediate Response
Given the rapid progression of symptoms, glioblastoma is often diagnosed after the sudden onset of neurological issues prompts immediate medical evaluation. Diagnostic steps include:
- Imaging: MRI and CT scans are typically used to visualize the tumor.
- Biopsy: A sample of the tumor tissue is analyzed to confirm the diagnosis.
Prognosis and Treatment
The prognosis for glioblastoma remains poor, with a median survival time of 12-15 months despite aggressive treatment. Treatment typically involves a combination of:
- Surgery: To remove as much of the tumor as possible.
- Radiation Therapy: To target residual cancer cells.
- Chemotherapy: Often with temozolomide.
- Experimental Treatments: Including clinical trials exploring new therapeutic approaches.
Conclusion
Glioblastoma is a highly aggressive and challenging type of brain tumor with a poor prognosis. It is relatively common compared to other brain tumors and primarily affects adults. The rapid progression of symptoms, including sudden neurological deficits and personality changes, underscores the need for prompt medical attention and comprehensive management strategies. While it may seem like I’m fighting against my brothers and sisters in Christ in the area of deliverance ministry, I am not. Understanding this disease (and many others) adds tools to our toolbox. This helps us (Christians) to aid our ailing neighbors and bring a quick end (or lead to treatment) to their suffering.
References
- American Brain Tumor Association. “Glioblastoma.” ABTA, https://www.abta.org/tumor_types/glioblastoma-gbm/.
- American Brain Tumor Association. “Personality Changes and Brain Tumors.” ABTA, https://www.abta.org/tumor_types/personality-changes-and-brain-tumors/.
- Brain Tumour Charity. “Cognitive and Personality Changes.” Brain Tumour Charity, https://www.thebraintumourcharity.org/living-with-a-brain-tumour/cognitive-and-personality-changes/.
- Lombard, A. J., et al. “Psychological Symptoms Associated with Glioblastoma Multiforme: A Literature Review.” Behavioral Sciences, vol. 10, no. 1, 2020, p. 13.
- Louis, D. N., et al. “The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.” Acta Neuropathologica, vol. 131, no. 6, 2016, pp. 803–820.
- Ostrom, Q. T., et al. “CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015.” Neuro-Oncology, vol. 20, suppl_4, 2018, pp. iv1–iv86.
- Stupp, Roger, et al. “Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma.” New England Journal of Medicine, vol. 352, no. 10, 2005, pp. 987-996.