For Christians and non-believers alike, understanding the medical basis for such conditions can help differentiate between physical illnesses and spiritual or demonic concerns.
Anti-NMDAR (N-methyl-D-aspartate receptor) encephalitis is a severe and potentially life-threatening autoimmune disorder that causes inflammation in the brain. This condition, characterized by a diverse array of psychiatric and neurological symptoms, can be particularly challenging to diagnose due to its overlap with primary psychiatric disorders. For Christians and non-believers alike, understanding the medical basis for such conditions can help differentiate between physical illnesses and spiritual or demonic concerns. This report delves into the causes, symptoms, diagnosis, and treatment of Anti-NMDAR encephalitis, supplemented by specific case studies to illustrate its complexity and severity.
Causes and Pathophysiology
Anti-NMDAR encephalitis occurs when the immune system produces antibodies against NMDA receptors in the brain. These receptors are crucial for synaptic transmission and plasticity, essential processes for learning and memory. The precise cause of this autoimmune response is not entirely understood, but it is often associated with tumors, particularly teratomas. These tumors can trigger the immune system to produce antibodies that mistakenly target NMDA receptors, leading to inflammation and disruption of brain function.
Symptoms
The symptoms of Anti-NMDAR encephalitis can be broadly categorized into psychiatric and neurological manifestations. These symptoms often overlap and can evolve rapidly, making early diagnosis and treatment critical.
Psychiatric Symptoms
The psychiatric symptoms of Anti-NMDAR encephalitis are diverse and can mimic a range of psychiatric disorders. These symptoms typically present early in the disease course and can include:
- Anxiety: Intense and irrational fears or worries.
- Paranoia: Delusions of persecution, such as believing others are plotting against the patient.
- Hallucinations: Auditory and visual hallucinations where patients hear voices or see things that are not there.
- Agitation and Aggression: Restlessness, irritability, or violent behavior without provocation.
- Catatonia: Marked decrease in movement and responsiveness, sometimes alternating with periods of hyperactivity.
- Behavioral Changes: Disorganized thinking, inappropriate behavior, and sudden personality changes.
Case Examples: Psychiatric Symptoms
- Case 1: Young Woman with Rapid Onset Psychosis
A 19-year-old woman presented with a sudden onset of psychiatric symptoms, including paranoia, auditory hallucinations, and bizarre behavior. Initially diagnosed with a primary psychiatric disorder and treated with antipsychotic medications, her condition worsened, leading to seizures and autonomic instability. High levels of anti-NMDA receptor antibodies were detected in her cerebrospinal fluid. Immunotherapy led to significant improvement in her psychiatric and neurological symptoms (Dalmau et al.). - Case 2: Adolescent Girl with Behavioral Changes
A 15-year-old girl was brought to the emergency department with a two-week history of behavioral changes, including aggression, inappropriate laughter, and mood swings. She exhibited catatonia and mutism. Initially thought to have a mood disorder, further testing confirmed anti-NMDA receptor antibodies. Aggressive immunotherapy and supportive care led to gradual improvement (Armangue et al.). - Case 3: Middle-Aged Man with Hallucinations and Delusions
A 45-year-old man experienced acute onset of auditory and visual hallucinations, believing he was being followed and that his family was in danger. Admitted to a psychiatric facility and treated for presumed psychosis, his symptoms persisted despite medication. He showed cognitive decline and motor abnormalities. Lumbar puncture confirmed anti-NMDA receptor antibodies. Immunotherapy resulted in a slow but steady recovery (Kayser & Dalmau).
Neurological Symptoms
Neurological symptoms often follow or accompany the psychiatric manifestations and can include:
- Seizures: Ranging from focal to generalized seizures.
- Movement Disorders: Involuntary movements such as orofacial dyskinesias, chorea, and dystonia.
- Memory Deficits: Short-term memory loss and difficulties in forming new memories.
- Speech Abnormalities: Aphasia, mutism, and echolalia.
- Autonomic Dysfunction: Irregular heart rate, blood pressure fluctuations, temperature regulation issues, and hypoventilation.
- Altered Consciousness: Fluctuations in consciousness, from confusion to coma.
- Sleep Disturbances: Insomnia or hypersomnia with disrupted sleep cycles.
Case Examples: Neurological Symptoms
- Case 4: Young Man with Recurrent Seizures
A 22-year-old man presented with recurrent seizures and confusion. Initially treated for epilepsy, his condition did not improve with standard antiepileptic drugs. He also developed psychotic symptoms and cognitive decline. MRI was normal, but CSF analysis showed anti-NMDA receptor antibodies. Treatment with immunotherapy, including corticosteroids and IVIG, significantly reduced seizure frequency and improved cognitive function (Dalmau et al.). - Case 5: Adolescent with Severe Movement Disorders
A 16-year-old girl developed sudden onset of involuntary movements, including orofacial dyskinesias and chorea, along with memory loss and speech difficulties. She became increasingly agitated and required sedation. MRI and EEG showed nonspecific abnormalities, but CSF analysis confirmed anti-NMDA receptor antibodies. Aggressive immunotherapy and plasma exchange led to the resolution of movement disorders and recovery of speech and memory functions (Armangue et al.). - Case 6: Middle-Aged Woman with Autonomic Instability
A 35-year-old woman was admitted with severe agitation, hallucinations, and autonomic instability, characterized by fluctuating blood pressure and heart rate, as well as hypoventilation requiring mechanical ventilation. She also exhibited catatonia and mutism. CSF analysis confirmed anti-NMDA receptor antibodies. Immunotherapy, including rituximab, cyclophosphamide, and supportive care, led to gradual stabilization and improvement in her symptoms (Titulaer et al.).
Diagnosis
Diagnosing Anti-NMDAR encephalitis involves a combination of clinical evaluation, laboratory tests, neuroimaging, and electroencephalogram (EEG).
- Clinical Evaluation: Assessment of symptoms and medical history.
- Laboratory Tests: Detection of anti-NMDA receptor antibodies in cerebrospinal fluid (CSF) and blood.
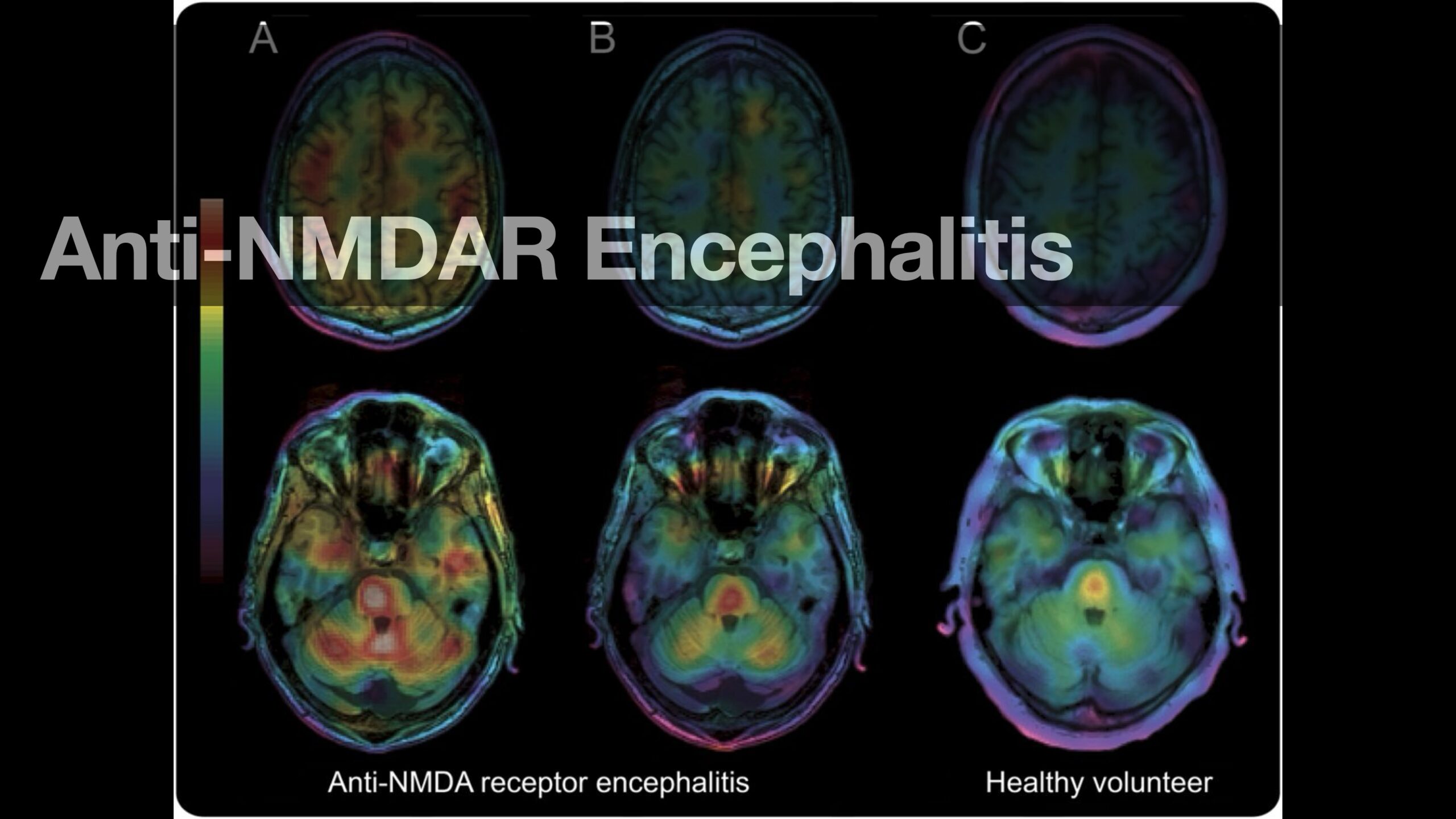
- Neuroimaging: MRI to identify inflammation or other abnormalities in the brain.
- EEG: To detect abnormal brain activity, which is common in this condition.
Treatment
The treatment of anti-NMDAR encephalitis typically involves immunotherapy and, if necessary, tumor removal. Early and aggressive treatment is crucial for improving outcomes.
- Immunotherapy: Includes corticosteroids, intravenous immunoglobulin (IVIG), plasma exchange, and rituximab or cyclophosphamide to reduce antibody production.
- Tumor Removal: Surgical removal of an underlying tumor, if identified, is crucial for improving outcomes.
- Supportive Care: Management of symptoms, such as anticonvulsants for seizures and medications for psychiatric symptoms.
Prognosis
The prognosis for Anti-NMDAR encephalitis varies. Many patients can recover fully or with minimal residual deficits with early and aggressive treatment. However, delayed treatment or severe cases can lead to significant neurological damage or be fatal. Long-term follow-up and rehabilitation may be necessary for some patients.
Final thoughts
Anti-NMDAR encephalitis is a complex and severe autoimmune disorder that presents with a wide range of psychiatric and neurological symptoms. Understanding these symptoms, along with proper diagnosis and treatment, is essential for distinguishing between medical conditions and potential spiritual or demonic issues. For Christians and non-believers alike, recognizing the medical basis for such conditions can help provide appropriate care and support for those affected.
References:
- Dalmau, J., et al. “Anti-NMDA-Receptor Encephalitis: Case Series and Analysis of the Effects of Immunotherapy.” Lancet Neurology, vol. 7, no. 12, 2008, pp. 1091-1098.
- Titulaer, M. J., et al. “Treatment and Prognostic Factors for Long-Term Outcome in Patients with Anti-NMDA Receptor Encephalitis: An Observational Cohort Study.” Lancet Neurology, vol. 12, no. 2, 2013, pp. 157-165.
- Armangue, T., et al. “Anti-NMDA Receptor Encephalitis in Children and Adolescents.” Annals of Neurology, vol. 76, no. 1, 2014, pp. 32-40.
- Kayser, M. S., and Dalmau, J. “Anti-NMDA Receptor Encephalitis in Psychiatry.” Current Psychiatry Reviews, vol. 7, no. 3, 2011, pp. 189-193.